Ligament Tears are a common injury people experience, especially with those who are active in sports. Yet, many of us are quite clueless while trying to imagine which of portion of the body it is that actually gets affected.
And rightly so, coz Ligaments aren’t a prominent body organ nor is it something that visible externally to the human eye. So, ignorance on this subject can be quite rational.
In this post lets learn more about Ligaments, get a bit well-versed in appreciating its functions and gain some understanding of what happens on someone has torn ligament injury.
What are Ligaments
Ligaments are fibrous and flexible tissues that connect our bones to other bones. They help to support the joints and allow a normal range of motion for the joints. Ligaments have high tensile strength due to the high density of collagen present. Ligaments also provide proprioceptive inputs to the brain and allow the body to perform complex activities required in sports.
Common Ligament Injuries
Injuries to the ligament are common in high impact (such as Badminton), high speed sports (especially athletics) with the knee and ankle being the most vulnerable. A structural damage to the ligaments is known as ligament sprains. There are some ligament injuries that are much more common than others and let’s take a look at them.
ACL Tears
Anterior Cruciate Ligament (ACL) injuries are common is high impact sports like football, soccer, rugby and basketball. The ACL is one of the 4 main ligaments in the knee which joins the femur to the tibia. Nearly 50% of patients who experience ACL injuries suffer it in combination with injuries to other parts of the knee such as the meniscus and medial collateral ligament.
ACL injuries occur most commonly from sudden twisting motion when the foot is still firmly planted on the ground while the knee is trying to change direction, causing the ACL to rupture. An ACL reconstruction will be the most viable option after injury as ligaments cannot heal by themselves.
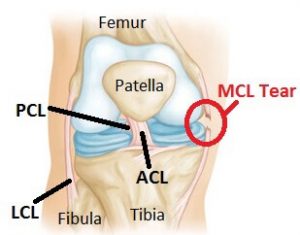 MCL Injuries
MCL Injuries
The medial collateral ligament (MCL) is another main ligament of the knee which provides stability to the knee. The MCL is located from the end of the femur to the top of the tibia and it prevents the knee from opening up. Due to its preventive features, it is commonly injured when there is an impact on the outside of the knee joint which causes the knee to buckle and the knee to open up.
MCL injuries are also mostly in conjunction with ACL and meniscus injuries. If it is a standalone MCL injury, surgery is often not required and patients can get on with their lives pretty well with the help of a knee brace to provide stability.
GHL Tears
The Glenohumeral joint ligaments (GHL) are located in the shoulders at the Glenohumeral joint which provides stability to the shoulder. The Glenohumeral joint connects the upper arm bone to the humerus and the shoulder blade. Injuries to the Glenohumeral joint occurs due to a fall and the patient landing on an outstretched arm, sudden twisting of the arm to beyond the normal motion range and a sudden impact on the shoulder, causing the ligaments to tear.
Above are 3 of the common ligament injuries that are experienced by many. Although ligaments are strong fibrous tissues, they can rupture if a sudden impact or twisting motion is applied on it. Ligaments are important in ensuring stability of the specific part of the body so extreme care should be taken to protect it.
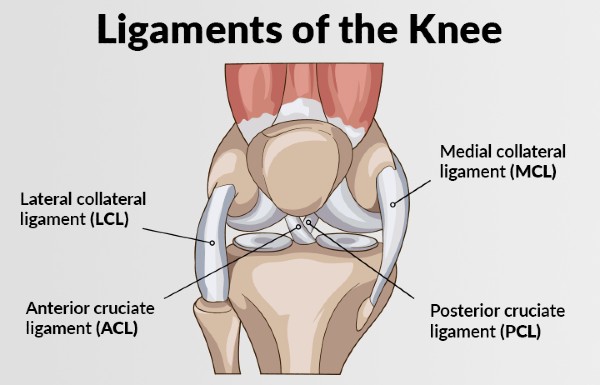
Symptoms & Treatments for Knee Ligament Tear
Our knee is supported by 4 main ligaments – anterior cruciate ligament (ACL), medial collateral ligament (MCL), lateral collateral ligament (LCL) and the posterior cruciate ligament (PCL). Each of the ligament plays a different role in ensuring the stability of the knee.
However, due to various reasons, the ligaments can be torn. Rupture of the ligament can be a partial one or a full one and this will affect the treatment administered. A ligament tear will also bring about instability in the knee and the inability for it to bear weight, causing problems when walking. In this article, we will look at some of the symptoms and treatments for ligament tears.
Common Symptoms
- As a general rule of thumb, a partially torn ligament will not bring about a pop sound while a fully ruptured one will produce a pop sound. A fully torn one can create instant instability and the knee may give way.
- Swelling occurs and the injured knee may start to turn purple due to the lack of proper blood flow to the area. Swelling occurs due to a build-up of blood from the injured ligament.
- The knee is unable to function properly, and you may feel that you are unable to control it.
- Tenderness will onset when you touch the knee.
Quick Care Options (for minor injuries)
- Protect the knee from further movements
- Resting the knee immediately following injury for at least 48 hours. If you need to move around, consider using crutches or walkers to prevent bearing weight on the injured knee.
- Ice will bring down swelling and reduce inflammation. Always try to ice the area every hour by using a cold compress or simply by wrapping knee in a towel and applying it locally.
- Compress the knee with a bandage to reduce swelling and prevent excessive movements.
- Elevate the knee to above your heart level to reduce swelling. This will cause excessive blood to flow away due to gravity towards your heart.
Treatment Options for Torn Ligaments
Here are the common treatment options for recovery from torn or ruptured Ligaments. The intensity of treatment needed and estimated knee sprain recovery time are dependent upon the severity of the injury.
- Physical Therapy: Strengthening the knee and its surrounding muscles, tendons, and ligaments can help to repair ligament injuries. Specific knee ligament injury treatment exercises can help to repair ligament damage and restore full function to the knee.
- Bracing: Wearing a knee brace or using crutches can help stabilize the knee and prevent sideways movements that may increase ligament damage and prevent healing and increase knee sprain recovery time.
- Surgery: For serious injuries or tears associated with other injuries normal healing may not help, in such cases your doctor will most likely recommend a surgical solution.
Nutrition Tips for Ligament Tear Recovery
The ligament is a fibrous tissue and its main function is to connect bones to another bone and prevent abnormal joint motions. Injuries to ligaments will take a long time to heal. However, good nutrition can help to speed up the recovery process. The vitamins and minerals in food can help to facilitate healing.
Proteolytic Enzymes: The first step of any injury is to reduce inflammation in the region and foods that contain Proteolytic enzymes are especially useful due to its anti-inflammatory properties which help to eliminate protein from the injured region. Foods that are rich in proteolytic enzymes include pineapples and ginger roots.
Zinc: Zinc is another mineral that is excellent in combating inflammation. The way our body works is fascinating. When one part of the body is injured, it will divert all the zinc in the body to the injured part to counter inflammation. As such, other parts of the body will have a zinc deficiency. In order to prevent zinc deficiency, it is important to consume foods that are rich in zinc such as oysters, wheat germ and veal liver.
Vitamin C: Vitamin C has excellent anti-inflammatory properties as well and when worked together with Proteolytic enzymes, it provides an even better result. Vitamin C is not a vitamin that they body can self synthesize. As such, patients will need to consume it in order for the body to possess it. Vitamin C is also required to produce collagen in the body and this is important in ligament healing. Foods that are rich in Vitamin C include citrus fruits, broccoli and tomatoes.
Protein: Protein is the building block of our body and it is required by the body for any healing process. Protein can easily be obtained from foods such as tofu, meat, eggs and soy products. Protein deficiency will lead to various ailments in the body.
Calories: Although the body’s metabolism is low during injury, there is still a need to consume sufficient calories on a daily basis. Calories are required in the healing process and if patients decide to cut down severely on their calorie intake, this will slow down the recovery process.
Ligament injuries will require physical therapy, surgery and proper nutrition to ensure a speedy recovery. Proper nutrition is not difficult to achieve. Although your movements will be severely limited, you can always ask a dear one to help you out in ensuring you receive sufficient nutrition daily.
Torn Ligament Treatment in Singapore
At the Singapore Sports and Orthopaedic Clinic, our orthopaedic specialists are ready to help you get back to the activities you know and love. Call us today for an appointment @ +65 6653 2981 to get a professional assessment of your condition & start your journey toward a better life!