
Why Referred Shoulder Pain should be a cause of concern to you
Feeling pain in any body part is never a desirable situation to be in. And when we do experience it the obvious reaction is treating
We produce orthopaedic-related recommendations, tips and updates from time to time. Be sure to check on this page regularly.

Feeling pain in any body part is never a desirable situation to be in. And when we do experience it the obvious reaction is treating

Ankle Sprains & Foot injuries are a common occurrence that can result while playing your favourite sport or maybe from a fall you experienced climbing

Our hips and knees undergo a lot of stress throughout our lives. These joints absorb substantial force and weight when we walk, jump, and move.

Ligament Tears are a common injury people experience, especially with those who are active in sports. Yet, many of us are quite clueless while trying

Looking for Orthopedic Bunion Corrector in Singapore? Let what Bunion Deformity Correction is first. Bunions & Bunionettes are a common cause of painful toes. A

Sprained ankles are one of the most common sports-related injuries obtained by people. Although a sprained ankle may not be a major injury, pain in

60-90% of the population will experience back pain in Singapore. Chances are you or someone you know has suffered from back pain at some point in
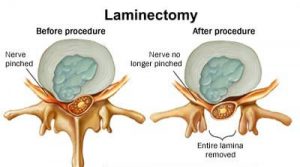
A laminectomy procedure on the lower back is one of the most common procedures to treat spinal stenosis, a narrowing of space around the spinal

Have you ever woke up to a stiff neck before? That uncomfortable and tight feeling that makes movement almost impossible and causing you a lot

Suffering from ankle pain when you’re trying to move can lead to less movement on your part. When you’re trying to stay in shape, get

If you suffer from knee pain or have had an injury to the knee, your doctor may suggest knee arthroscopy to see what is going

When it comes to everyday life your feet play a huge role. They take you from one place to the next, help you get where

Our clinic offers same day appointment, X-ray/MRI facilities, Insurance filing services and amenities like pharmacy store & wheelchair accessibility.
© Singapore SPORTS and Orthopaedic Clinic

